
Learn how diabetic retinopathy is diagnosed, treated, and managed. This guide covers key treatments and how assistive tools like IrisVision can support those living with vision loss.
Diabetic retinopathy is a complication of diabetes that affects the eyes. Over time, high blood sugar can damage the small blood vessels in the retina. The retina is the part of the eye responsible for sensing light. This damage can lead to vision problems and, if left untreated, may result in permanent vision loss.
The condition often develops silently. It can affect people with type 1 or type 2 diabetes, especially those who have had diabetes for several years or struggle to manage their blood sugar levels.
There are different stages of diabetic retinopathy. In early stages, the changes may be minor and go unnoticed. In more advanced stages, new and abnormal blood vessels may grow and leak, causing more serious damage. As the condition progresses, everyday tasks like reading, recognizing faces, or walking safely may become more difficult.
For a deeper overview of the causes and stages, see IrisVision’s guide on diabetic retinopathy:
Diabetic Retinopathy – Exploring the Basics
Detecting diabetic retinopathy early is one of the most important steps in preventing vision loss. Since the condition often begins without noticeable symptoms, regular eye exams are essential for anyone living with diabetes.
Eye care professionals use several tests to examine the retina and assess any damage:
Dilated Eye Exam
This is the most common test. Eye drops are used to widen the pupil, allowing the doctor to see the retina more clearly. They check for swelling, bleeding, or abnormal blood vessels.
Optical Coherence Tomography (OCT)
This imaging test provides detailed cross-sectional images of the retina. It helps detect fluid buildup, swelling, or early structural changes.
Fluorescein Angiography
A special dye is injected into a vein in the arm. As the dye travels through the blood vessels in the eye, a camera captures images to show any leakage or abnormal growth.
These tests are safe and usually completed during a routine eye exam. Early detection allows for timely treatment and better outcomes.
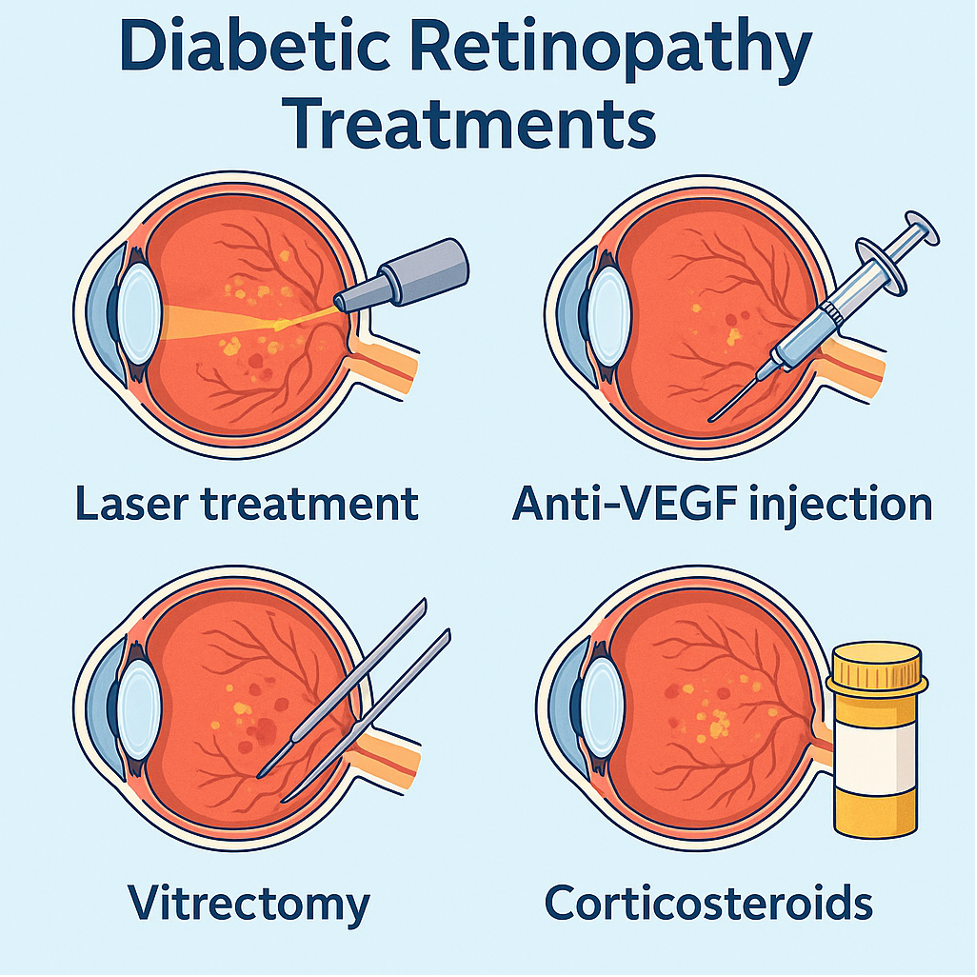
The goal of treating diabetic retinopathy is to stop or slow the progression of damage to the retina and preserve as much vision as possible. Treatment depends on the stage of the disease, whether there is swelling in the retina, and if new, abnormal blood vessels have formed.
For many patients, early-stage diabetic retinopathy may not require immediate medical intervention. But once the disease progresses or begins to affect vision, one or more of the following treatments may be recommended.
Before any eye-specific treatment is considered, managing the underlying diabetes is critical. This includes:
Maintaining good systemic control can slow the progression of diabetic retinopathy and reduce the risk of developing complications like diabetic macular edema (DME), a swelling of the retina that can cause vision loss.
Anti-VEGF (vascular endothelial growth factor) medications are currently the most common treatment for diabetic retinopathy with macular edema or abnormal blood vessel growth.
These medications are injected directly into the eye, usually once a month in the beginning. Over time, the frequency may be reduced based on the patient’s response.
Common anti-VEGF drugs include:
How they work:
They block a protein that triggers the growth of abnormal blood vessels in the retina. This helps reduce swelling, prevent bleeding, and protect central vision.
What to expect:
The injection is performed under local anesthesia and takes only a few minutes. Many patients notice stabilization or improvement in vision after a few treatments, though regular follow-up is necessary.
For patients who do not respond well to anti-VEGF therapy or are unable to continue it, corticosteroid injections may be considered. These reduce inflammation and swelling in the retina.
Steroids may be delivered in two forms:
While effective in reducing macular edema, steroids carry a higher risk of side effects, including elevated eye pressure and cataract development. Eye pressure must be monitored closely.
Laser therapy has been used for decades in the treatment of diabetic eye disease. Although anti-VEGF injections are more common now, laser remains an important tool in certain cases.
Types of laser treatment:
How it works:
The laser targets areas of the retina to seal off leaks or reduce oxygen demand in the retina, which can help stop abnormal vessels from growing.
What to expect:
Laser treatment is usually done in a clinic setting. It may cause mild discomfort or blurry vision for a short time, but it helps reduce long-term risks of severe vision loss.
In advanced stages of diabetic retinopathy, where there is bleeding (vitreous hemorrhage), retinal detachment, or extensive scar tissue, surgery may be necessary.
Vitrectomy is a procedure that removes the gel-like vitreous inside the eye and replaces it with a clear fluid or gas. It also allows the surgeon to remove scar tissue and repair the retina.
When is it recommended?
Recovery:
Patients may need to position their head a certain way after surgery, depending on the technique used. Vision may take weeks or months to improve.
Tailored Treatment Plans and Follow-up Care
Each case of diabetic retinopathy is unique. Eye doctors will recommend a treatment plan based on several factors including:
Most treatment plans also require frequent follow-ups. Regular monitoring is important to track progress, catch new changes early, and adjust care as needed.

Diabetic retinopathy can change the way you experience the world. As the condition progresses, even after treatment, some level of vision loss may remain. While medical interventions aim to slow or stop the damage, many people still need long-term support to adapt to their changing vision.
This is where low vision care becomes essential.
Diabetic retinopathy can change the way you experience the world. As the condition progresses, even after treatment, some level of vision loss may remain. While medical interventions aim to slow or stop the damage, many people still need long-term support to adapt to their changing vision.
This is where low vision care becomes essential.
Understanding the Impact of Vision Loss
Vision loss from diabetic retinopathy can affect daily routines and emotional well-being. People may find it difficult to:
These challenges are common, and adjusting to them takes time. But with the right support, many people find new ways to live fully and independently.
Low vision rehabilitation is a process that helps individuals make the most of their remaining sight. It is not about curing vision loss but about learning to live with it effectively.
Rehabilitation often involves:
A low vision specialist typically leads this process. They assess your vision, lifestyle, and goals, then recommend tools and strategies tailored to your needs.
There are a range of tools available for people with diabetic retinopathy. These include:
These aids allow people to regain access to tasks they may have stopped doing—like reading, writing, watching TV, or navigating unfamiliar places.
To explore more about these tools, see IrisVision’s guide here:

IrisVision is a wearable low vision aid developed in collaboration with vision experts and medical institutions. It is designed to support people with conditions like diabetic retinopathy by enhancing their usable vision in real time.
The latest version, IrisVision Live 2.0, offers an even more refined and accessible experience. It combines wide-field magnification with personalized viewing modes, making it easier to adapt to different environments and tasks.
With IrisVision Live 2.0, users can:
The device is lightweight, easy to use, and designed to be worn comfortably for extended periods. It does not restore lost vision, but it can make the most of what remains, helping people live with greater independence and confidence.
Many individuals with diabetic retinopathy already rely on IrisVision as part of their vision care plan. It serves not only as a tool, but also as a bridge back to everyday life.
Diabetic retinopathy can feel uncertain and overwhelming, but it does not have to define your future. With regular eye exams, proper diabetes management, and timely medical treatment, many people are able to protect and preserve their vision.
For those who experience vision changes, support is available. Low vision rehabilitation, assistive tools, and wearable technologies like IrisVision Live 2.0 can help you stay connected to the people, places, and routines that matter most.
If you or someone you care about is living with diabetic retinopathy, know that you are not alone. With the right care and tools, it is possible to adapt and continue living a full, independent life.
Support
See and Connect Today!
IrisVision Global, Inc.
5994 W. Las Positas Blvd, Suite 101
Pleasanton, CA 94588
Email: [email protected]
Support: +1 855 207 6665
Support
See and Connect Today!
IrisVision Global, Inc.
5994 W. Las Positas Blvd, Suite 101
Pleasanton, CA 94588
USA Email: [email protected]
Support: +1 855 207 6665
Support
See and Connect Today!
IrisVision Global, Inc.
5994 W. Las Positas Blvd, Suite 101
Pleasanton, CA 94588
Email: [email protected]
Support: +1 855 207 6665